While we are not at that point just yet, that does not mean there is not some massively exciting work happening in the field, however. The latest example? Research carried out at Georgia Institute of Technology and the Piedmont Heart Institute in Atlanta, where investigators have created 3D-printed heart valves, designed for use in the planning of lifesaving surgeries.
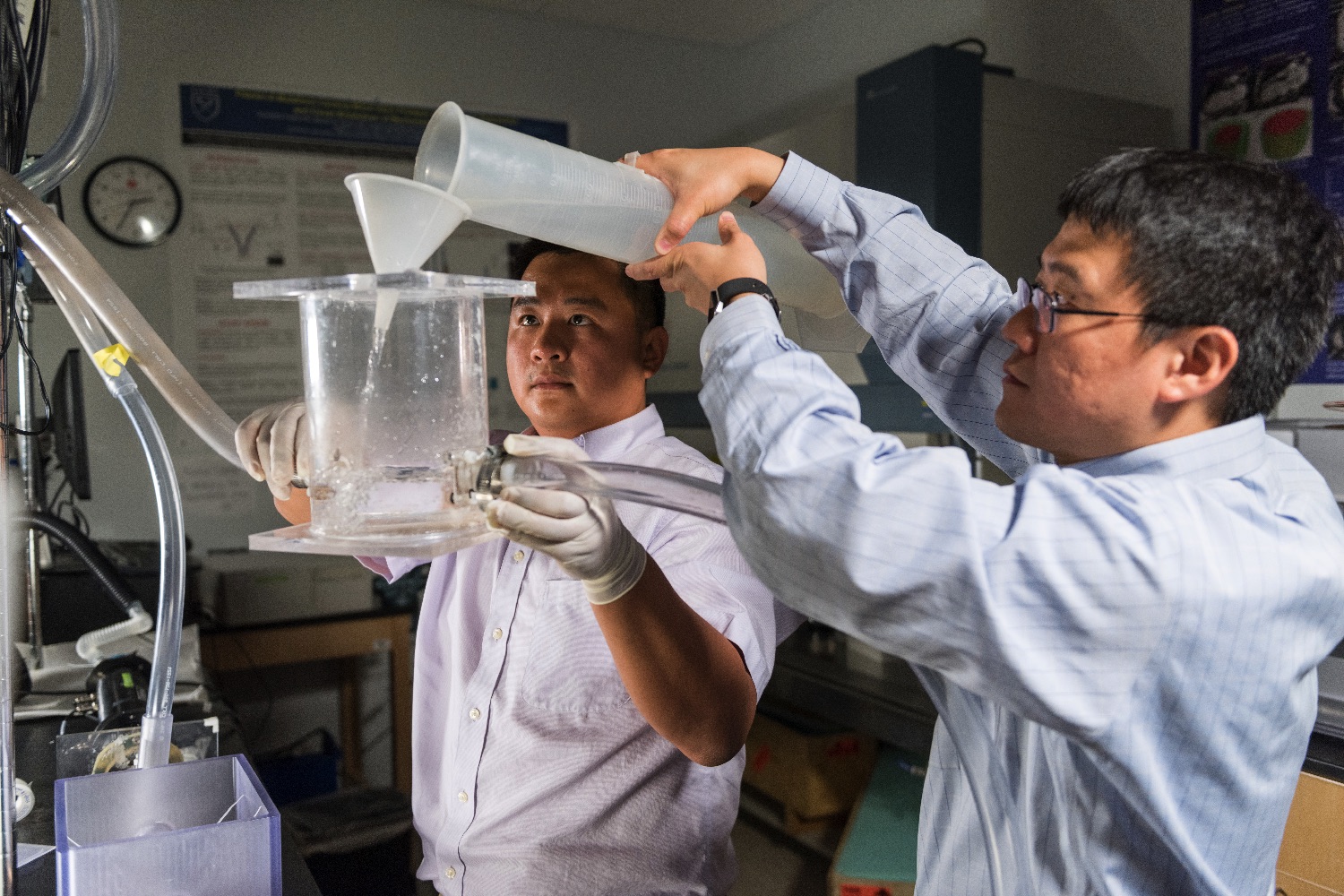
“The Georgia Tech and Piedmont Heart Institute team has developed an integrated materials design and 3D-printing technique for making heart valves that can closely mimic human heart valve functions,” Georgia Tech engineering professor Chuck Zhang told Digital Trends. “These 3D-printed valves can be used by doctors or surgeons for surgery planning, such as selecting the most matching prosthetic valve, and determining the location of the stent to be inserted in the aortic valve in a transcatheter aortic valve replacements (TAVR) procedure.”
As with other applications of 3D printing, the big advantage of the technology here is the high level of customization it offers. Replacement valves which don’t fit properly can cause leakage-related complications, potentially resulting in the death of the patient. By creating 3D-printed models from CT scans of patients’ hearts, cardiologists will be able to test valve models for fit prior to surgery taking place.
So far, the researchers have done in vitro testing of the technology retrospectively on 18 patients. Although these patients had received previous heart valve replacements, the researchers were able to manufacture 3D-printed valves and study them to see how well they functioned in test conditions. The study showed that the 3D-printed valves were able to predict not only the occurrence of post-TAVR (transcatheter aortic valve replacement) paravalvular leaks, but also its location and severity.
“The next step is to further refine the technique and perform more tests,” Zhang said. “We also plan to work with companies to commercialize this technique so that it can be available for surgeons to use in related operations in the near future.”
The work is described in a paper published in the journal ACC: Cardiovascular Imaging.