The bioreactor uses cell-free protein synthesis (CFPS) technology which allows for the production of proteins without a living system. The team of researchers applied the idea of CFPS and condensed it down into a microfluidic bioreactor that can be used wherever the medicine is needed. “The fact it’s cell-free reduces the infrastructure needed to produce the protein and opens the possibility of creating proteins when and where you need them, bypassing the challenge of keeping the proteins cold during shipment and storage,” said ORNL lead scientist Scott Retterer.
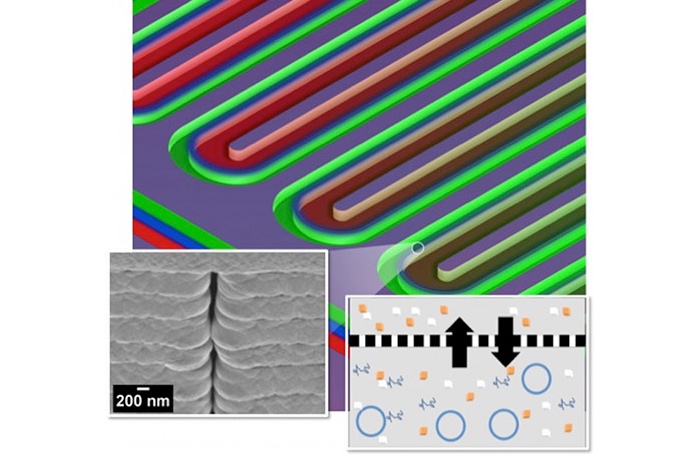
The bioreactor itself is comprised of two parallel silicon channels 16 feet in length that are coiled together in a snake-like fashion inside the device. One channel is the feeder side and contains the chemicals for the reaction, while the other channel is the reactor side and serves as a chamber for the chemical reaction. The two channels are separated by a porous nanofabricated membrane that allows for the exchange of metabolites, energy, and other reaction components. The nature of the material makes it easy for scientists to modify the size of the membrane’s pores and control the exchange of chemicals. These modifications give scientists complete control over the reaction times, enabling them to optimize protein yields.
Besides convenience, this on-demand reactor has the advantage of producing drugs on a small and affordable scale. It theoretically can be used to synthesize drugs, such as personalized medicines and orphan drugs, that typically are too expensive to mass produce. Retterer, along with colleague Mitchel Doktycz and others, have been working on this technology for more than a decade with funding provided by DARPA, the National Institutes of Health, and the Department of Energy.



